Pre-Payment Review Results for Emergent Ambulance Services for January to March 2025
Pre-Payment Review Results for Emergent Ambulance Services for Targeted Probe and Educate (TPE) for January to March 2025
The Centers for Medicare & Medicaid Services (CMS) implemented the TPE process for Healthcare Common Procedure Coding System (HCPCS) codes A0427 and A0429 for Emergent Ambulance Services. The reviews with edit effectiveness are presented here for Alabama, Georgia and Tennessee.
Cumulative Results
| Number of Providers with Edit Effectiveness | Providers Compliant Completed/Removed After Probe | Providers Non-Compliant Progressing to Subsequent Probe | Providers Non-Compliant/Removed for Other Reason |
|---|---|---|---|
| 10 | 6 | 4 | 0 |
| Number of Claims with Edit Effectiveness | Number of Claims Denied | Overall Claim Denial Rate | Total Dollars Reviewed | Total Dollars Denied | Overall Charge Denial Rate |
|---|---|---|---|---|---|
| 262 | 66 | 25% | $125,678.62 | $29,448.25 | 23% |
Probe One Findings
| State | Number of Providers with Edit Effectiveness | Providers Compliant Completed/Removed After Probe | Providers Non-Compliant Progressing to Subsequent Probe | Providers Non-Compliant/Removed for Other Reason |
|---|---|---|---|---|
| Ala. | 3 | 1 | 2 | 0 |
| Ga. | 3 | 2 | 1 | 0 |
| Tenn. | 4 | 3 | 1 | 0 |
| State | Number of Claims with Edit Effectiveness | Number of Claims Denied | Overall Claim Denial Rate | Total Dollars Reviewed | Total Dollars Denied | Overall Charge Denial Rate |
|---|---|---|---|---|---|---|
| Ala. | 80 | 26 | 33% | $35,875.02 | $10,848.03 | 30% |
| Ga. | 59 | 20 | 34% | $27,801.91 | $9,056.31 | 33% |
| Tenn. | 123 | 20 | 16% | $62,001.69 | $9,543.91 | 15% |
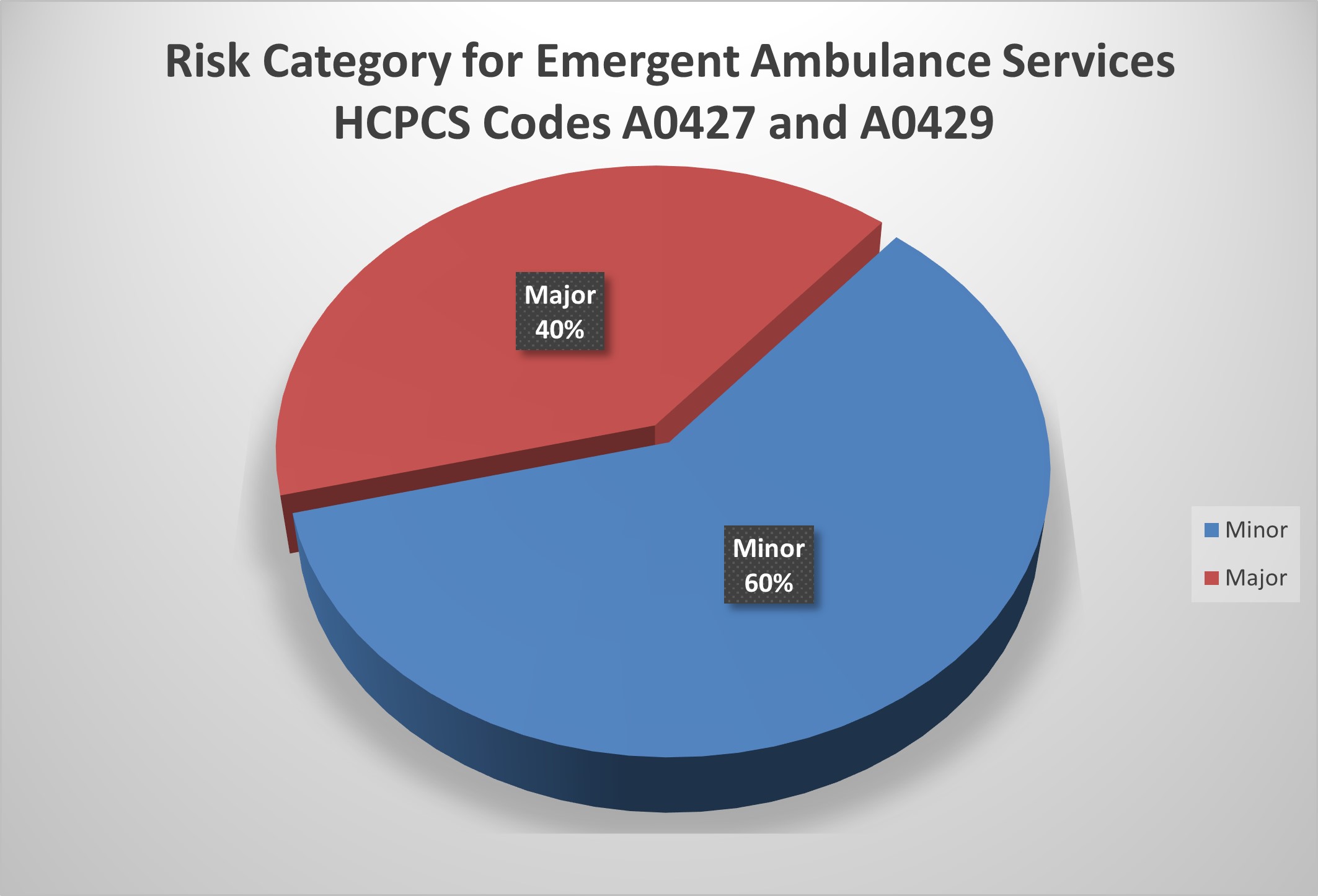
Risk Category
The risk categories for HCPCS codes A0427 and A0429 Emergent Ambulance Services are defined as:
| Risk Category | Error Rate |
|---|---|
| Minor | 0–20% |
| Major | 21–100% |
Figure 1. Risk Category for Emergent Ambulance Services HCPCS Codes A0427 and A0429.
Top Denial Reasons
| Percent of Total Denials | Denial Code | Denial Description | Number of Occurrences |
|---|---|---|---|
| 44% | BNSIG | Documentation Received Lacks the Necessary Beneficiary or Authorized Representative Signature | 7 |
| 31% | NODOC | Documentation Requested for this Date of Service Was Not Received or Was Incomplete; Therefore We Are Unable to Make a Reasonable and Necessary Determination as Defined Under Section 1862(a) (1) (A) of the ACT for the Service Billed, and this Service Has Been Denied | 5 |
| 19% | WRONG | Documentation Received Contains an Incorrect, Incomplete or Illegible Patient Identification or Date of Service | 3 |
| 6% | NOTMN | Payer Deems the Information Submitted Does Not Support the Medical Necessity of the Services Billed | 1 |
Denial Reasons and Recommendations
BNSIG — Documentation Received Lacks the Necessary Beneficiary or Authorized Representative Signature
- Review documentation prior to submission to ensure that the proper beneficiary or authorized representative signature is included and is legible
- For illegible signatures, clearly print or type the full name of the owner of the signature
NODOC — Documentation Requested for this Date of Service Was Not Received or Was Incomplete; Therefore We Are Unable to Make a Reasonable and Necessary Determination as Defined Under Section 1862(a) (1) (A) of the ACT for the Service Billed, and this Service Has Been Denied
- Submit all documentation related to the services billed within 45 days of the date on the Additional Documentation Request (ADR) letter
- Review documentation prior to submission to ensure that the documentation is complete and that all dates of service requested are included
- Include any additional information pertinent to the date of service requested to support the services billed. For example: original chart notes, diagnostic, radiological or laboratory results.
- For claims denied with a M127 or N29 code listed on the remittance advice, be sure to submit all documentation for all dates of service on that claim with a reopen/redetermination request form by fax to JM Part B (803) 699–2427, JJ Part B (803) 870–0139 or Railroad Beneficiary Appeals (803) 462–2218
WRONG — Documentation Received Contains an Incorrect, Incomplete or Illegible Patient Identification or Date of Service
- Review all documentation prior to submission to ensure that it is for the correct patient and date of service
- Ensure that patient identifiers are legible and complete
- Ensure that the complete date of service is clearly and legibly noted on all documentation
- Prior to billing claims, review the information to determine that the correct patient identifier and the correct date of service are listed in the appropriate field
NOTMN — Payer Deems the Information Submitted Does Not Support the Medical Necessity of the Services Billed
- Ensure that all documentation to support medical necessity of the service billed is submitted for review. This includes original chart notes and any diagnostic, radiological or laboratory results.
- Verify that documentation to support the level of service billed is included. Please refer to Palmetto GBA's for links to applicable Local Coverage Determinations (LCDs), National Coverage Determinations (NCDs) and the Evaluation and Management (E/M) Scoresheet Tool for documentation requirements.
Education
Palmetto GBA offers providers selected for TPE an individualized education session to discuss each claim denial. This is an opportunity to learn how to identify and correct claim errors. A variety of education methods are offered such as webinar sessions, web-based presentations or teleconferences. Other education methods may also be available. Providers do not have to be selected for TPE to request education. If education is desired, please complete the Education Request Form (PDF).
Next Steps
Providers found to be non-compliant (major risk category/denial rate of 21–100 percent) at the completion of TPE Probe 1 will advance to Probe 2, and providers found to be non-compliant (major risk category/denial rate of 21–100 percent) at the completion of TPE Probe 2 will advance to Probe 3 of TPE after at least 45 days from completing the 1:1 post-probe education call date.